our projects
Research
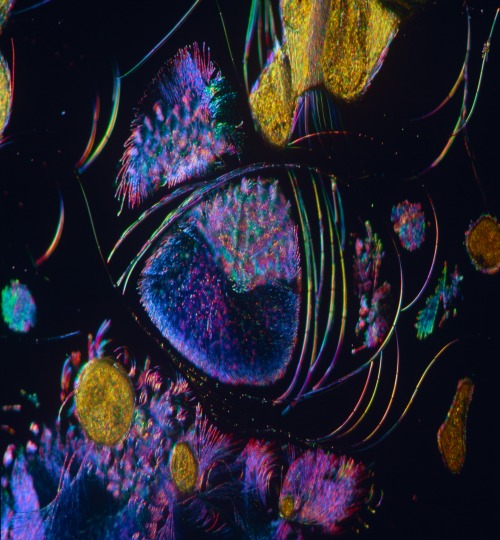
Dysimmune Diseases Foundation (DDF) funds research into the cause, treatment, and cure for autoimmune diseases.
CURRENT AND PROSPECTIVE RESEARCH
2021 DYSIMMUNE DISEASE FOUNDATION YOUNG INVESTIGATOR RESEARCH GRANT

DDF Young Investigator Research Grant
Award: $75,000 over 2 Years
Immunologic Phenotyping of Patients with Neuromuscular Immune-related Adverse Events after Checkpoint Inhibitor Therapy
Dysimmune Diseases Foundation is pleased to announce the recipient of the DDF 2021 Young Investigator Research Grant.
Leeann Burton, MD, at Massachusetts General Hospital Department of Neurology, has been awarded the grant for her research “Immunologic Phenotyping of Patients with Neuromuscular Immune-related Adverse Events after Checkpoint Inhibitor Therapy”.

Dr. Sohail Masood, founder of Dysimmune Diseases Foundation, recently met with Dr. Burton to discuss her research and extend his congratulations. “I am delighted that DDF can support emerging clinical research like Dr. Burton’s” said Dr. Masood. “The intent of the Young Investigator Research Grant has been realized in helping fund her research, and it has been a pleasure to talk with her about her work. DDF is proud to encourage new avenues of clinical research in autoimmune neuromuscular disease through this grant designed for investigators in the early stages of their careers. Ultimately, the goal of DDF is to support autoimmune disease patients and the research that can help understand and treat their disease.” In agreement, Dr. Burton adds that she is “honored to be the first recipient of the Young Investigator Research Grant. This grant will fund work that is critical to advancing our ability to optimally predict risk, diagnose, and treat patients with neuromuscular complications of checkpoint inhibitor therapies. Additionally, I am thankful to the Dysimmune Disease Foundation for this early funding opportunity, which will help me build my career in academic medicine. “
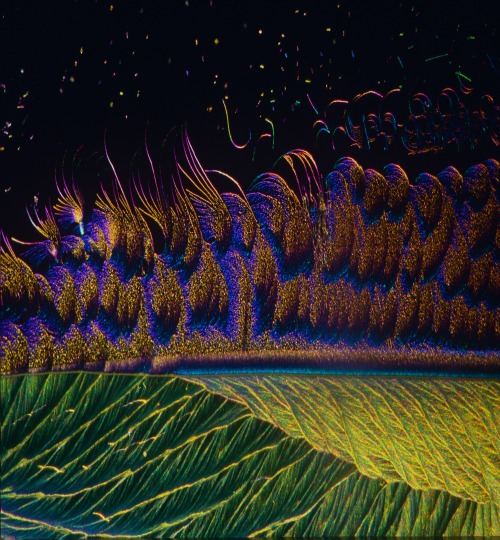
AUTOIMMUNE DERMATOLOGIC DISEASES
BULLOUS DISEASE
Bullous diseases are rare autoimmune disorders that cause painful blistering and erosion of the skin and mucous membranes. This group of diseases include bullous pemphigoid, dermatitis herpetiformis, epidermolysis bullosa acquisita, linear immunoglobulin A disease, mucous membrane pemphigoid, pemphigoid gestationis, pemphigus foliaceus, and pemphigus vulgaris. These diseases may be treated with corticosteroids, immunosuppressant agents, and IVIG. The supported research below discusses current and emerging treatment paradigms and associated risks and benefits.
SUPPORTED RESEARCH
- Kaveri S, Ahmed AR. Reversing Autoimmunity: Combination of Rituximab and Intravenous Immunoglobulin. Frontiers in Immunology. (Front. Immunol. 9:1189. doi: 10.3389/fimmu.2018.01189)
- Yanovsky R, McLeod M, Ahmed AR. Treatment of pemphigus vulgaris: part 1 – current therapies. (Expert Review of Clinical Immunology. 2019;15:1047–1060)
- Yanovsky R, McLeod M, Ahmed AR. Treatment of pemphigus vulgaris: part 2 – emerging therapies. (Expert Review of Clinical Immunology 2019;15:1061–1071)
- Kridin K, Ahmed AR. Post-rituximab immunoglobulin M (IgM) hypogammaglobulinemia. (Autoimmunity Reviews. 2020 Mar;19(3):102466.
- Kridin K, Ahmed AR. Anti-p200 Pemphigoid: A Systematic Review. (Front. Immunol. 10:2466. doi: 10.3389/fimmu.2019.02466)
Ongoing research
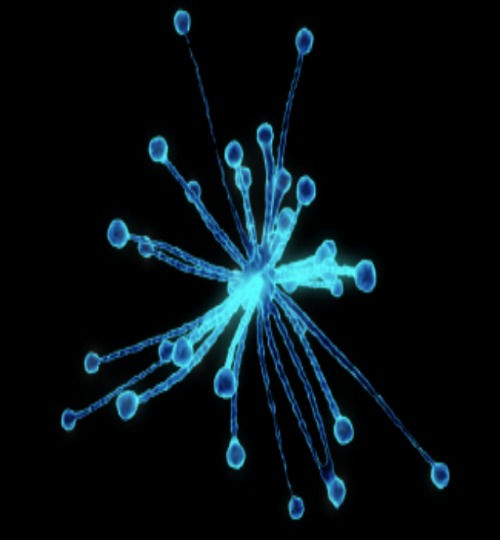
INFLAMMATORY NEUROPATHY WITH DIABETES MELLITUS (DM)
Finding the Efficacy of IVIG in Patients with Dysimmune Neuropathy and Diabetes (FIND-IVIG), an observational registry study
Distal symmetric polyneuropathy is the most common neuropathy to occur in diabetes mellitus (DM), but patients with DM can also develop inflammatory neuropathies, the most common of which is chronic inflammatory demyelinating polyradiculoneuropathy (CIDP).1 The amenability
of CIDP, an immune-mediated neuropathy, to treatment with immunoglobulin (IG), makes its identification important.1-3 There is a growing body of evidence suggesting that the prevalence of CIDP tends to be higher in patients with DM.3 CIDP is the most treatable neuropathy that can occur with DM, and the rapidly progressive disability caused by CIDP and other inflammatory neuropathies warrants awareness among healthcare professionals of the potential benefit of immunomodulatory therapy in patients with such afflictions.1 There is a need for heightened awareness of inflammatory neuropathy associated with DM in order to promote earlier diagnosis and treatment with IVIG. The purpose of this observational study is to prospectively collect data related to responsiveness to IVIG treatment in patients with inflammatory/demyelinating neuropathies with DM, and compile and analyze clinical data against a comparator group of patients without DM.



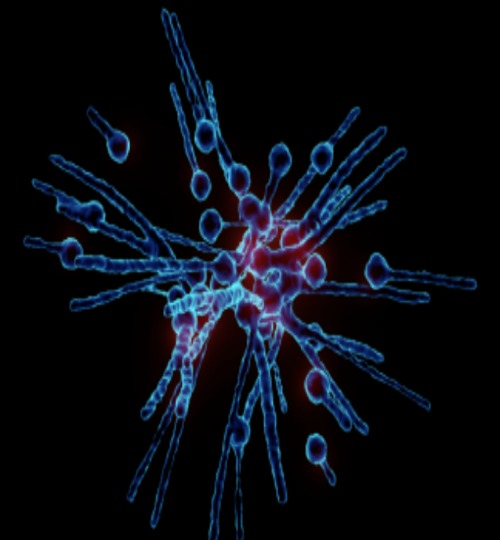
Prospective Research
Finding the Efficacy of IVIG in Apparently Autoimmune Small Fiber Neuropathy (FIND-IVIG-aaSFN)
with Diabetes, an observational registry study
Peripheral neuropathy is a significant public health concern that affects nearly 40 million individuals in the United States 1 . Small fiber neuropathy (SFN) is the most common cause of neuropathic pain in peripheral neuropathies and may elicit debilitating pain in patients. 2 The etiology of SFN may be diverse and include autoimmune causation for a subset of patients. Whether this also extends to a subset of patients with diabetes is not fully explored. 3,4 Though limited data about the treatment of such patients exists, the reported efficacy of treatment of intravenous immunoglobulin (IVIG) makes it clinically important to identify aaSFN patient subsets (i.e., those with an underlying autoimmune pathomechanism). 5 There is a need for heightened awareness of aaSFN patients among practicing neurologists to promote earlier diagnosis, identify autoimmune causes and consider the benefit of immunomodulatory therapies, including treatment with intravenous immune globulin (IVIG). The purpose of this observational study is to prospectively collect data related to responsiveness to IVIG treatment in patients with aaSFN with diabetes or prediabetes, and compile and analyze clinical data against a comparator group of aaSFN patients without diabetes.